
Two bioactive ingredients in cannabis have been found to have antifungal properties when applied topically, according to a groundbreaking new study. The discovery comes as the World Health Organization urgently calls for new treatments for potentially deadly fungal infections.
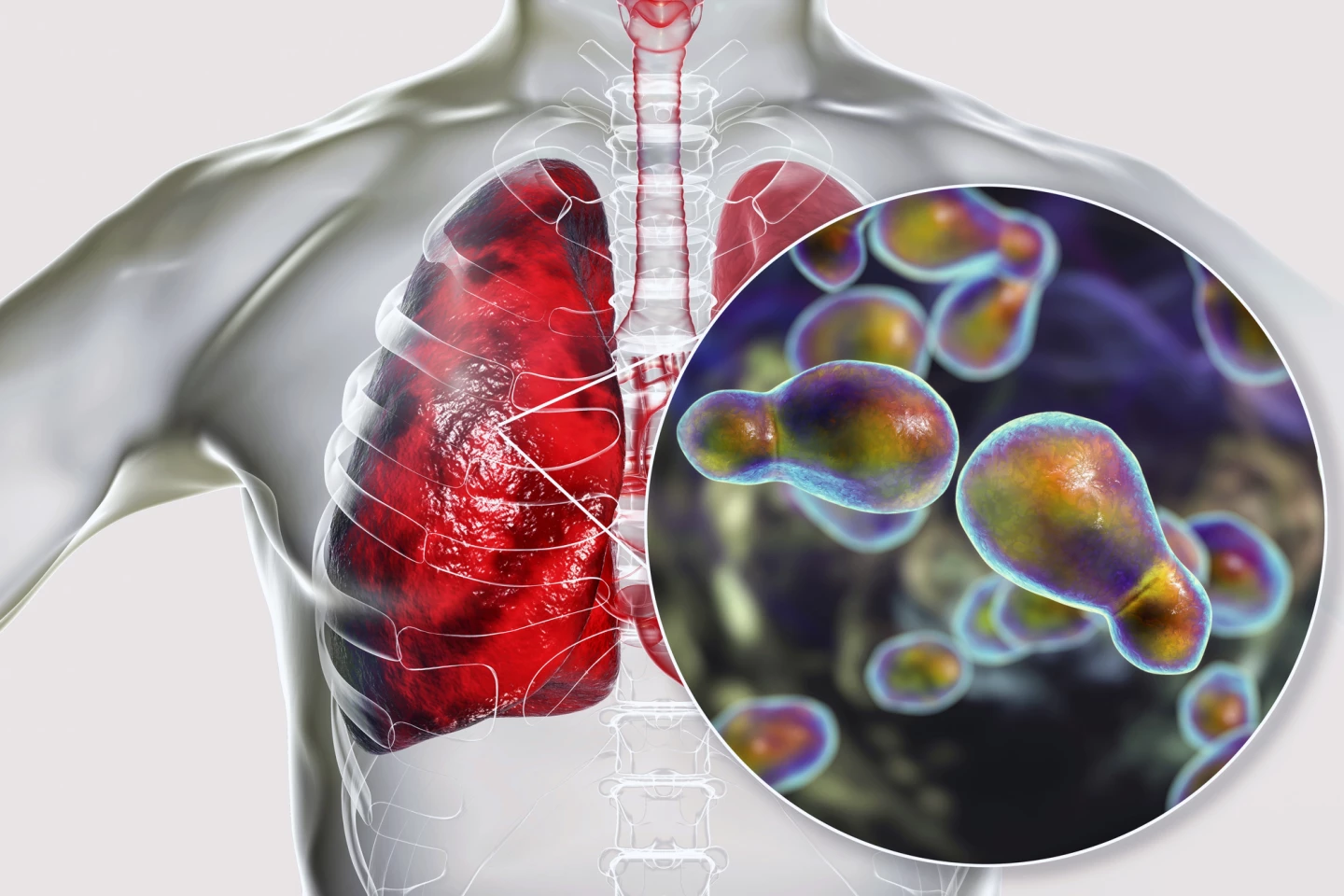
We often hear about the threats of bacterial and viral infections, but less frequently about those of fungal infections. But that doesn’t mean they’re less of a problem. For the first time ever, the World Health Organization (WHO) recently reported on the urgent need for improved tests and treatments for fungal infections and listed the potentially deadly Cryptococcus neoformans as a priority.
New research led by Australia’s Macquarie University has demonstrated that two of the bioactive ingredients in cannabis, the cannabinoids cannabidiol (CBD) and cannabidivarin (CBDV), have impressive antifungal properties when used topically.
“When Cryptococcus neoformans gets to your nervous system, it causes life-threatening meningitis,” said Dr Hue Dinh, the study’s lead author and a postdoctoral research fellow in Macquarie’s School of Natural Science. “Hundreds of natural compounds can be extracted from the cannabis plant, and we don’t know which ones work.”
Invasive fungal infections, such as those caused by Candida or Cryptococcus, cause around 3.8 million deaths annually. As is the case with antibiotics, there is a growing worldwide resistance to antifungal drugs that poses a risk to human health. WHO’s report on antifungal drugs, published in April 2025, points out that in the past decade, only four antifungal medications have been approved by the US Food and Drug Administration (FDA), the European Medicines Agency (EMA), or the Chinese National Medical Products Administration.
CBD is the second most prevalent active ingredient in cannabis, derived from the hemp plant, that doesn’t cause a high and isn’t considered addictive. CBDV, which is also non-intoxicating, is less studied (and, therefore, less well-known) than its media-exposed counterparts, CBD and cannabis’ main psychoactive compound, tetrahydrocannabinol (THC). But like CBD, its potential as a medical treatment continues to be explored.
Cannabinoids-as-antifungals are an attractive proposition given their safety profile in humans and the fact that they’ve already been approved to treat a number of conditions, including epilepsy, nausea, and chronic pain. A few previous studies have shown that cannabis extracts containing a mixture of natural cannabinoids have antifungal properties against particular fungi. So, the researchers set out to assess the antifungal activity of CBD and CBDV against C. neoformans, specifically, and across a broader spectrum of Cryptococcus species, as well as other clinically significant fungi. They also hoped to elucidate the mechanism of action of the two cannabinoids in fighting C. neoformans.
The researchers tested the fungus-killing abilities of different concentrations of CBD and CBDV on C. neoformans to determine the minimum fungicidal concentration (MFC). This concentration was then used to ascertain the time-dependent effect of both cannabinoids. By 30 minutes after treatment, both CBD and CBDV had rapidly killed off the fungus. When they combined the cannabinoids with existing antifungal drugs – fluconazole and amphotericin B – the researchers noted no synergistic or antagonistic effect; the cannabinoids didn’t seem to interact with the drugs.
To assess the broad antifungal effects of the cannabinoids, the researchers tested them against 33 fungal strains, including pathogens designated by the WHO as critically important, as well as diverse strains from veterinary, clinical, and environmental sources. They found that CBD and CBDV were effective against a range of Cryptococcus strains and tinea-causing fungi. They were less effective or ineffective against Candida strains, suggesting that the pair are not as broad-spectrum as the researchers had hoped.
In terms of the mechanism of fungicidal action, through protein analysis, the researchers were able to ascertain that CBD and CBDV disrupted cell membranes and metabolism. This is important information. Interfering with cell membranes and not cell processes means it’s harder for microbes to develop resistance to cannabinoids through mutations or adaptation. They can’t easily evolve to repair a broken membrane like they can an altered cellular process. In addition, the cannabinoids disrupted biofilm formation, which is crucial to C. neoformans’ survival because it shields the fungus from the body’s immune system.
Finally, as a proof-of-concept study, the researchers tested the effectiveness of topical CBD as an antifungal to treat C. neoformans in living insects. They used greater wax moth (Galleria mellonella) larvae, which are often used as a model for studying fungal infections because these moths share many similarities with mammals’ antifungal immune system. Infected larvae treated with topical CBD had survival rates that were near those of uninfected larvae, indicating that CBD could be used as a topical antifungal in the clinical setting.
The study’s findings are promising. Future research is needed to assess the effectiveness of CBD and CBDV, which are molecularly similar but exhibit different antifungal activities, in animals, including humans.
“If we can demonstrate that these ones work well for common infections, you could actually just get some CBD oil and then rub it on your skin to treat it,” Dinh said.
The study was published in the journal PLOS Journal of Neglected Tropical Diseases.
Source: Macquarie University








